New York, NY — It is the end of a long afternoon. You arrive home, relax, and begin to plan your upcoming day. Instead of working tomorrow, you must make your monthly trip to the clinic. As you pack your bag in preparation for tomorrow’s journey, you envision the day ahead: walking miles across town; waiting on the long line for hours; meeting with nurses for a quick check up; and waiting again at the pharmacy for your medications. You begin to feel the weight of making up for lost time at work.
The Price of Success
The scale-up of HIV treatment is one of the world’s great public health success stories. The number of people accessing ART in low and middle-income countries has increased rapidly, and an estimated 7.8 million deaths have been prevented.
With patients now living longer and treatment-for-all approaches being adopted in many countries, demand for treatment has grown rapidly and people living with HIV are accessing services in unprecedented numbers. The United Nations has adopted ambitious 90–90–90 targets that aim to identify 90 percent of individuals with HIV, initiate 90 percent of those diagnosed on ART, and maintain viral suppression in 90 percent of those on treatment.
Achieving these ambitious targets will not be easy. It will require a near doubling of the number of people on treatment despite several stark realities, including flat funding for HIV programs, overcrowded health facilities, and program data that point to gaps in quality such as sub-optimal patient retention rates.
A Paradigm Shift in HIV Care
Global health experts believe they have identified a solution that will help countries reach the 90–90–90 goals. Differentiated service delivery, also known as differentiated care, moves away from a one-size-fits-all approach, enabling stable patients to access treatment closer to the community, and freeing up space at clinics and treatment centers. By tailoring the frequency and location of services available to different groups of patients, as well as the type of health worker providing those services, differentiated service delivery aims to enhance the quality and efficiency of health services and to improve patient satisfaction. Key elements of this approach have been endorsed by the WHO, PEPFAR, and the International AIDS Society. An increasing number of national ministries of health are supporting a need to re-assess the “when, where, who, and what” of HIV services for patient groups with different clinical, psychosocial, and contextual characteristics.
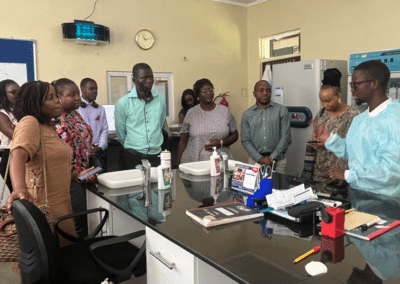
To help accelerate the implementation of differentiated service delivery in sub-Saharan Africa, ICAP is launching an ambitious three-year project called the HIV Coverage, Quality and Impact Network (CQUIN), funded by the Bill & Melinda Gates Foundation. The project will convene a network of ministries of health from countries across sub-Saharan Africa, as well as leaders in HIV program design and policy, to help countries take differentiated care to scale. The goal is to encourage south-to-south exchange and experience sharing among members through ongoing communication and learning opportunities. Through CQUIN, ICAP will also provide support and expert guidance to generate new information and new models of differentiated service delivery.
“At its core, CQUIN is designed to be a learning network,” notes Dr. Miriam Rabkin, director for health systems strategies at ICAP. “The goal is to support countries to work together to take differentiated service delivery to scale,” adds Dr. Peter Preko, CQUIN’s project director: “The network will enable countries to share experiences, innovations, and best practices so they can move differentiated care from pilot projects to national programs.”