DSD
Differentiated service delivery (DSD) is a person-centered approach to HIV prevention, testing, and treatment. Moving away from a one-size-fits-all model, DSD tailors HIV services to diverse groups of people living with HIV while maintaining the principles of the public health approach to enable high-quality service delivery at scale.

Why Differentiated Service Delivery?
Changing global guidelines and ambitious prevention, testing, and treatment targets have markedly increased the number of people eligible for HIV services. At the same time, global funding for HIV has plateaued, and many countries are being asked to do more with less regarding HIV programming.
In addition, gaps in program quality and service delivery models that do not meet the needs and expectations of people living with HIV threaten both individual outcomes and public health goals.
Differentiated service delivery is a practical approach to addressing these challenges.
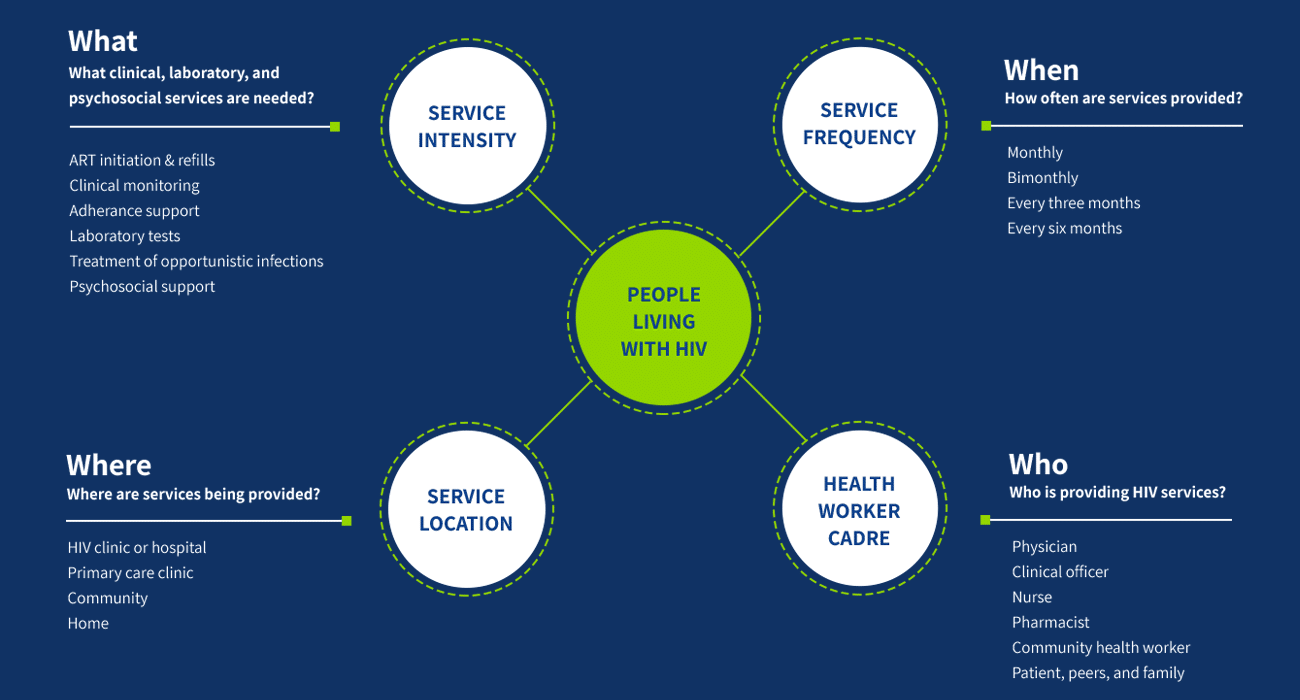
DSD varies the design and delivery of services offered to different groups and aims to enhance quality, efficiency, and recipient of care satisfaction. The goal is to place individuals at the center of service delivery while maximizing health system efficiency. Key elements of this approach include re-assessing the “when, where, who, and what” of HIV services for groups with different clinical, psychosocial, and contextual characteristics.
How it Works
Differentiated service delivery varies the “when, where, who and what” of service delivery to create models that respond to different needs, contexts, and groups of people. The 21 countries in the CQUIN network have tailored DSD models to their settings; these are described on each country page.
Learn more about DSD at:

Differentiated HIV Treatment
Differentiated antiretroviral therapy (DART) includes more-intensive service delivery models for people newly starting HIV treatment, those with opportunistic infections and/or co-morbidities, people with unsuppressed viral load, groups who typically need close follow-up such as children, adolescents, and pregnant people, and those with psychosocial barriers to adherence and retention.
DART also includes innovative less-intensive service delivery models for people doing well on ART. Less-intensive DART models include facility-based and community-based approaches, each of which may be provided in individual or group settings by health care workers or peers. These models typically emphasize education and empowerment of recipients of care, streamlined services, and less frequent visits to health facilities.
In addition to making HIV treatment more convenient and person-centered, DSD allows health workers to spend more of their time with people needing more intensive services, increasing efficiency and improving quality of care.
ICAP’s CQUIN team worked with network stakeholders to develop a capability maturity model for differentiated treatment, which describes the key domains needed for ministries of health to deliver high-quality DART at scale.
Differentiated HIV Testing and Linkage
Differentiated HIV testing services (dHTS) leverage the “when, where, who, and what” approach to provide testing services, using the status-neutral testing framework. Status-neutral testing services provide equal emphasis on linking people who test positive to HIV treatment and on linking people who test negative and are at high risk of HIV acquisition to HIV prevention services.
In 2022, ICAP’s CQUIN team worked closely with the Clinton Health Access Initiative (CHAI), Ministries of Health, the World Health Organization, PEPFAR, the South-to-South Learning Network, and other partners to conceptualize a capability maturity model for HIV testing and linkage services. Ministries of health now have access to this tool, which contains key domains to assess their national HIV testing programs.

Differentiated HIV Prevention
Differentiated HIV prevention focuses on preventing new HIV infections, improving health outcomes for recipients of care living with HIV, and reducing HIV-related health inequities by providing comprehensive and simplified PrEP services.
Learn more: WHO guidelines on simplified and differentiated service delivery of pre-exposure prophylaxis (PrEP), 2022
Learn more about status-neutral HIV prevention and care