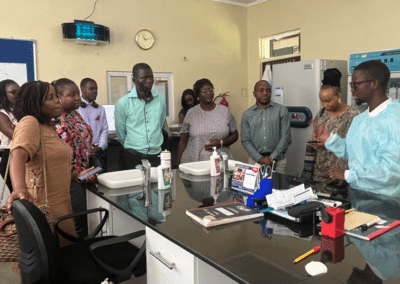
New York, NY — As HIV programs expand at a rapid pace, health systems around the world are working hard to keep up. New global guidelines and strategies have markedly increased the number of people living with HIV who are eligible for treatment. This has created exciting new opportunities to control the epidemic, but is also straining the capacity of health facilities, health workers, and the systems in which they operate.
In response, a new approach to HIV program design – differentiated service delivery – has been developed as a way to improve both the quality and efficiency of HIV programs. Through its HIV Coverage, Quality, and Impact Network (CQUIN), ICAP is helping to lead the charge toward a new future of high quality, high impact, and sustainable HIV programs.
Differentiated service delivery – also called differentiated care when referring to care and treatment – is a relatively new concept with great promise for enhancing the coverage, quality, and impact of HIV services. CQUIN is a bold initiative that will foster joint learning about differentiated service delivery across multiple countries in sub-Saharan Africa. The three-year project is about more than an exchange of ideas. Its focus on joint learning is grounded in an ambitious vision: By 2020, CQUIN countries will have taken differentiated service delivery to scale, improving individual health and achieving population-level impact.
One cross-cutting challenge will be identifying the best way to measure the scale-up and spread of differentiated service delivery, which is not presently captured by traditional monitoring and evaluation (M&E) approaches. ICAP is working with network partners to develop systems and tools for routine M&E of differentiated service delivery. To understand the baseline in each network country, the CQUIN team has also developed an innovative dashboard tool to describe where countries are along the continuum of differentiated service delivery implementation.
Using nine domains, the dashboard will enable stakeholders to summarize progress towards scale-up of differentiated services. Once piloted and validated, the tool can be used by diverse stakeholders, from ministries of health to civil society, to characterize a baseline and track changes over time.
“The dashboard was developed after our initial discussions with CQUIN member countries,” says Dr. Miriam Rabkin, CQUIN’s principal investigator. “We realized there was no common language to describe the scale-up and spread of differentiated services, and that the CQUIN learning network is a great forum for joint-development of such a tool.”
“The dashboard is in final draft stage,” noted Dr. Peter Preko, CQUIN’s project director. “We’ll be seeking additional feedback and suggestions at our upcoming CQUIN meetings, as part of our validation and implementation strategy.”
The CQUIN team welcomes feedback to improve the dashboard. Email us with your suggestions.