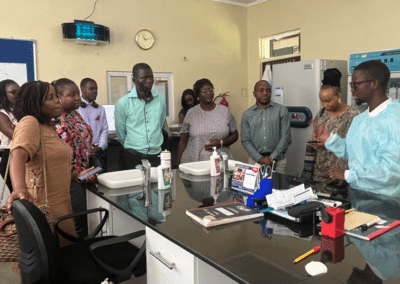
HIV testing is critical to achieving epidemic control and the UNAIDS 2030 targets. To support ministries of health and stakeholders to expand HIV testing services in Africa, CQUIN, recently convened over 200 stakeholders to share knowledge, best practices, and innovations in delivering person-centered HIV testing and linkage services.
“Although most CQUIN partner countries have made great strides in scaling up HIV treatment, the percentage of people who know their status is far too low in many settings,” said Miriam Rabkin, MD, MPH director for health systems strategies at ICAP. “HIV testing coverage is a critical barrier to achieving both treatment and prevention goals, and the combination of new testing strategies and new testing technologies makes this a good time for country teams to share lessons learned and think about ways to accelerate progress.”

CQUIN hosted the Differentiated Service Delivery Across the HIV Testing Cascade meeting from March 13 to 16 in Nairobi, Kenya. Participants included ministry of health representatives from 22 countries and stakeholders from global organizations, including the World Health Organization (WHO), UNAIDS, the Global Fund, PEPFAR, the U.S. Centers for Disease Control (CDC), the US Agency for International Development (USAID), the Clinton Health Access Initiative (CHAI), the International AIDS Society (IAS), FHI 360, the International Treatment and Preparedness Coalition (ITPC), and the Bill & Melinda Gates Foundation. Through CQUIN, ICAP supports ministries of health to advance and scale up differentiated HIV treatment and testing services to improve health outcomes and strengthen health systems by convening learning exchange meetings, supporting country-to-country visits, supporting targeted data collection, and providing a wide range of other technical assistance activities.
At this meeting, participants presented case studies in implementing differentiated service delivery (DSD) for HIV testing services (HTS), with a focus on status-neutral testing services that provide equal emphasis on linking people who test positive to HIV treatment and on linking people who test negative and are at high risk of HIV acquisition to HIV prevention services. The meeting addressed mobilization and demand creation, innovative ways to deliver HTS, and the key issues of linkage to prevention, linkage to treatment, and linkage to re-engagement for individuals who have interrupted treatment services. Presentations included dHTS as a Gateway for Linking to Services, Applying Community-led Monitoring to HIV Testing, Linkage from Testing to Prevention and Treatment Services, and many more.
Country representatives also shared results and lessons learned from national self-assessments of testing services at the health system level, using CQUIN’s latest tool, the Differentiated HIV Testing Services Capability Maturity Model (dHTS CMM), to assess their national HIV testing programs.
“The dHTS capability maturity model enables countries to identify diversity, gaps, and challenges in their national HIV testing programs,” said Peter Preko, MBChB, CQUIN project director, in an interview after the meeting. “For instance, 16 out of 21 countries who used the dHTS CMM to assess how well their programs were doing ahead of the meeting found gaps in monitoring and evaluating testing services. This is an area where CQUIN will prioritize joint learning and co-creating solutions among countries in the network.”

For almost half of the meeting participants (45 percent), this was the first time attending a CQUIN meeting, and for most of them, the meeting was an eye-opener. Several participants were intrigued by the concept of a status-neutral approach to HIV programming.
“I thought the status-neutral approach shared in one of the meeting presentations was a very interesting way for ministries of health to expand HIV programming,” said Joyce Murerwa, MBBS, a senior prevention officer with the Rwanda Biomedical Association attending a CQUIN meeting for the first time. “The case studies on PrEP scale-up in Liberia, Zimbabwe, and South Africa, and triple elimination of syphilis, hepatitis, and HIV in pregnant women, were also a few highlights for me,” she added.
“The knowledge exchange opportunities provided at the meeting exposed us to untapped opportunities to mobilize, test, and link our key and vulnerable populations to their status-specific interventions,” said Raphael Adu-Gyamfi, MD, MPH, DSD coordinator at Ghana’s National AIDS/STI Control Program. “Our team has realized that it is possible to achieve epidemic control with a little more effort, and we are encouraged, as a program, to improve our outputs with the lessons learned. We look forward to working more closely with stakeholders to improve comprehensive client care in Ghana.”
On the final day of the meeting, eight countries presented action plans for improving and scaling up HIV testing services in their countries. All 22 countries developed these action plans and activities throughout the meeting through country-to-country group discussions and single-country sessions.
“We plan to improve and revise our monitoring and evaluation tools,” said Fatou Fall, MD, HIV Counselling and Testing lead at Senegal’s National AIDS Control Program, in her presentation. “Currently, Senegal does not have guidelines, which support monitoring recipients of care who we link to PrEP, for instance.”
In the following months, CQUIN will work with partners, including CHAI, to support ministries of health and learning among countries in the network as they develop solutions to the gaps identified in their HIV testing programs.
“We have plans to launch an HIV testing services community of practice in May and to schedule quarterly calls to discuss cross-cutting dHTS gaps and brainstorm relevant solutions,” said John Bosco Matovu, MBChB, MPH, MSc, CQUIN regional clinical advisor who leads the HTS stream of work. “Furthermore, CQUIN will host webinars on topics prioritized by country teams, including status-neutral testing, the use of digital platforms to improve demand creation for HIV self-testing, linkage to combination prevention services after HIV testing, target setting for HIV testing, social network testing, and more.”
All meeting presentations and resources are available here: https://cquin.icap.columbia.edu/event/differentiated-service-delivery-across-the-hiv-testing-cascade/