In the past several years, countries in the CQUIN network have scaled up access to less-intensive differentiated service delivery (DSD) models for people living with HIV. An assessment of four CQUIN-supported DSD performance reviews (DPRs) conducted in 2022 shows a gradual increase in the enrolment and retention of recipients of care in differentiated treatment models such as community antiretroviral therapy (ART) groups, multi-month ART dispensing, ART adherence clubs, and other models for people doing well on ART.
“In most CQUIN partner countries, routine program data provide only a limited window into the implementation and scale up of differentiated treatment models. In this context, DPRs are a unique opportunity for countries to conduct in-depth assessments of DSD program performance and a strategy to facilitate in-country DSD learning exchange to promote scale-up of quality DSD,” said Karampreet Sachathep, PhD, ICAP’s senior strategic information manager and assistant professor of Population and Family Health at the Columbia Mailman School of Public Health. “The data show us that countries have effectively scaled up less-intensive treatment models over the years, and that people in these models are retained in care and doing well,” she added.
Two of the most recent DPRs found that people who had been on ART for 36 months were 50% and 100% more likely to be enrolled in less-intensive models (LIM) compared to people who had been on ART for 12 months. Data from another DPR showed that a cohort of people on ART followed over three years showed a gradual increase in LIM enrollment from 38% in 2020 to 66% in 2021 to 79% in 2022. A fourth DPR also showed a gradual rise in LIM enrollment in one cohort from 35% in 2020 to 40% in 2021 and to 53% in 2022.
Comparing people enrolled in LIM models versus those enrolled in more intensive models (MIM) and outcomes among those retained in each model for at least 12 months, one DPR showed that 93% and 91% of people in MIM (who had not transferred out) were alive and on ART at 24 months and 36 months, respectively. In contrast, 98% and 96% of people in LIM were alive and on treatment at 24 and 36 months.
“Given that the eligibility criteria for LIM require people to be doing well on treatment, it is not surprising to see that outcomes such as retention and viral load suppression are superior,” said Dr. Sachathep. “However, these data are often not routinely available to ministries of health, and DPRs provide countries an opportunity to dig much deeper to find gaps and opportunities to learn from the successful implementation of differentiated treatment models.”
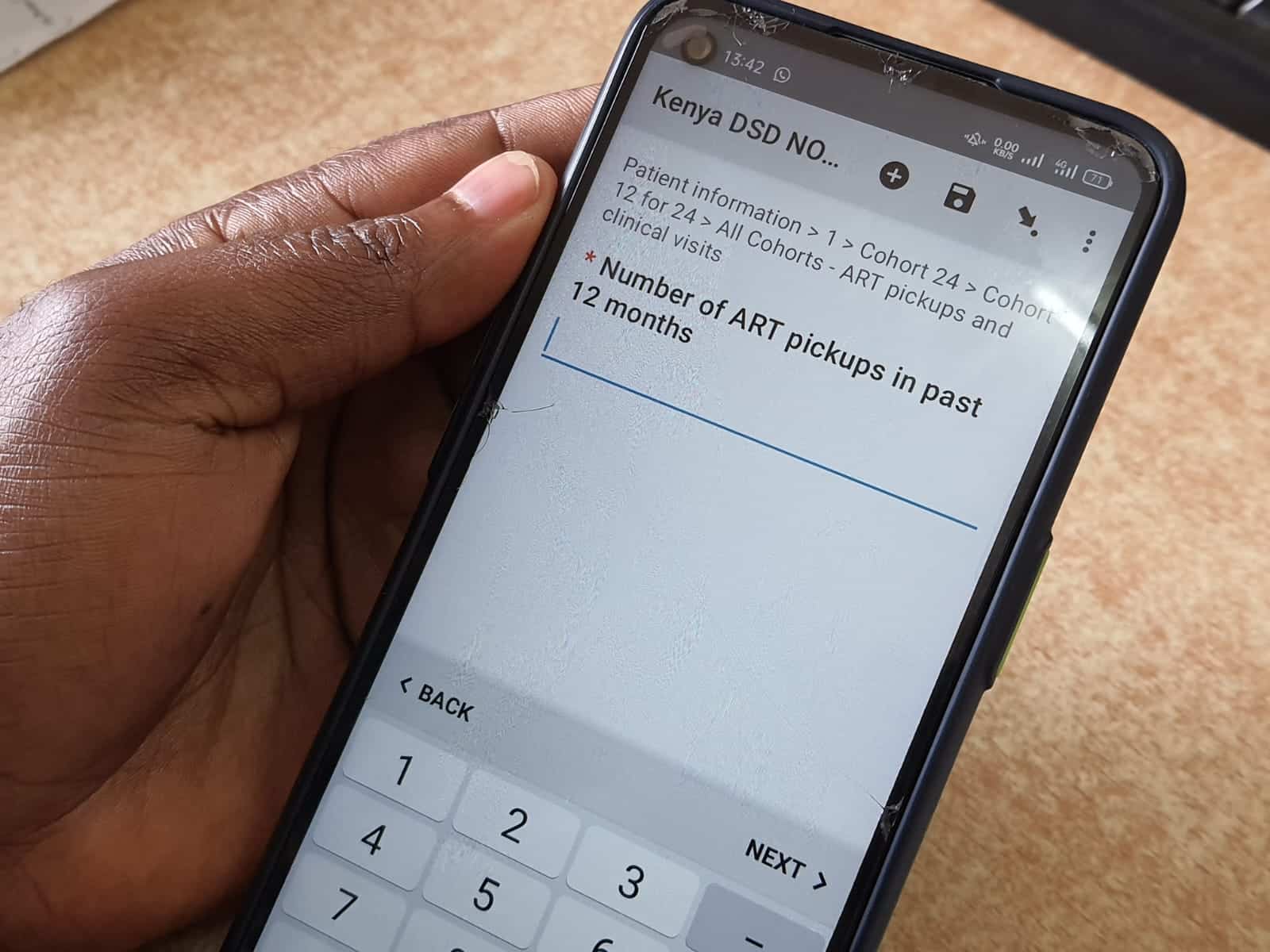
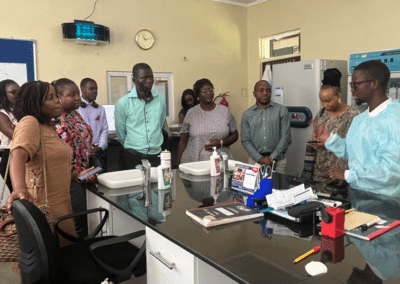
DPRs involve targeted collection and analysis of routine, existing patient-level information enabling ministries of health to assess DSD program implementation in ways that are not otherwise possible in most contexts. The ICAP CQUIN team worked with diverse stakeholders in the Differentiated M&E Community of Practice to develop a detailed DPR toolkit that can be adapted for diverse country contexts. All DPRs are led by ministries of health, who tailor the DPR approach to address national priorities. Through CQUIN, ICAP provides technical and financial support for primary data collection, data analysis, development of data visualizations, and presentation of the results at in-person workshops where stakeholders, including ministries of health, donors such as the United States President’s Emergency Plan for AIDS Relief (PEPFAR), civil society, care providers, and implementing partners discuss the findings and develop action plans.
“One benefit of the DPR is that it provides an opportunity to get snapshots of DSD program performance across time and learn lessons as ministries of health gradually update national M&E systems to eventually provide much of this kind of data,” said Bill Reidy, PhD, MPH, ICAP’s Deputy Director for Strategic Information.
CQUIN has helped to roll out 19 DPRs since 2018, with sample sizes varying from a little over 1000 participants to over 7000. Data collection is scheduled for four more countries in the upcoming months. “Since its inception, partner countries have used the DPR results dissemination platform for in-country learning exchange and cross fertilization of best practices,” said Peter Preko, MBChB, MPH, CQUIN project director. “The action plans developed at the dissemination meetings help countries to address DSD implementation gaps identified through the DPRs,” he added.
“The DSD Performance Review in Kenya was a country-led activity funded mostly by PEPFAR-Kenya, with ICAP/CQUIN technical assistance support and funding for non-PEPFAR supported counties”, said Rose Wafula, MPH, head of Kenya’s National AIDS and STI Control Program, NASCOP. “The DPR has provided very useful data at country and facility levels that revealed our successes and gaps and will inform targeted quality improvement activities as we roll out and implement DSD at scale for various sub-populations.”
“The DPRs have demonstrated the critical role DSD has played in assessing quality across the continuum of HIV care and treatment,” said Cordelia Katureebe, MBChB, HIV Care and Treatment coordinator at Uganda’s Ministry of Health AIDS Control Program. “The patient level chart reviews conducted through these DPRs are a continuum of the national quality improvement initiative and will be key for sustainability.”
“DPRs provide an opportunity for Ministry of Health staff to enhance their knowledge and skills in conducting rigorous DSD program evaluation,” said Werner Maokola, MD, head of the Strategic Information Unit, National AIDS Control Program, Ministry of Health Tanzania. “We will use the findings to inform our HIV programming.”