The CQUIN network in collaboration with the South-to-South Learning Network (SSLN) convened over 800 people including representatives of ministries of health, recipients of care, donors, implementers, academics, and advocates to discuss the critical importance of scaling up high-quality prevention, testing, care and treatment services for key populations in Africa.
The goal of the four-day virtual meeting was to share current policy, science, and guidance, foster the exchange of best practices, and support partner countries to improve the quality and coverage of HIV services for key population groups, including sex workers, men who have sex with men, transgender people, and people who inject drugs.
“Key populations are disproportionally affected by HIV in all epidemic contexts,” said Cassia Wells, MD, MPH, senior technical advisor for CQUIN and key population community of practice lead. “Key populations and their sexual partners accounted for 62 percent of new HIV infections in 2019 so HIV prevention, testing, and treatment efforts tailored to these groups is essential for epidemic control,” she said.
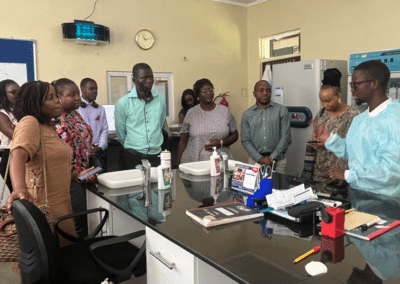
Access to the key population meeting content, including slide presentations, videos, questions and answers from meeting discussions, as well as pictures of the in-country watch meetings, are available to view here on the CQUIN website.
Highlights
Plenary Sessions: Inequalities, the Future of HIV Prevention for Key Populations, and More
In her opening keynote presentation, Shannon Hader, MD, MPH, UNAIDS deputy executive director for programs, highlighted the inequalities and disparities faced by members of key population groups in accessing health care services. According to Hader, creating opportunities for differentiated HIV services for key populations, including fostering an enabling social and legal environment, are essential steps countries and stakeholders need to make to achieve epidemic control. The opening plenary also featured contributions from Wafaa El-Sadr, ICAP global director, Bernard Madzima, CEO of Zimbabwe’s National AIDS Council, Magreth Kagashe from the Tanzania Ministry of Health, and Grace Kamau from the African Sex Workers Alliance.
Other plenary sessions explored differentiated prevention, testing and treatment services for key populations, data for decision making to guide key population programs, creating enabling environments for HIV service delivery for key population groups, and the use of virtual interventions to support HIV services along the cascade.
In the 10 parallel sessions, presenters showcased diverse case studies, best practices, and resources for prevention, testing, linkage, and treatment tailored for key population groups. Examples include:
Implementing a Community-Based PWID-led Needle and Syringe Program in Nigeria
Aniedi Apkan, executive director of the Drug-Free and Preventive Healthcare Organization, DAPHO in Nigeria, presented a case study on a pilot project on needle and syringe exchange for people who inject drugs, DAPHO in collaboration with other partners implemented in three states. Akpan detailed the process from project planning to project launch in this session on Differentiated HIV Models for Key Populations.
Reducing Stigma Toward Key Populations in Eswatini
Bheki Sithole, the technical advisor for FHI 360 in Eswatini, showcased lessons learned and next steps in the program’s Meeting Targets and Maintaining Epidemic Control (EpiC) project intervention in the country. In his presentation, Sithole depicted how the EpiC project engaged stakeholders using several strategies, including conducting an integrated bio-behavioral surveillance study, sensitizing law enforcement and health care workers, and forming a technical working group to reduce stigma in Eswatini – a critical barrier preventing key populations from accessing HIV services.
DSD Models for Transgender People
This session’s goal was to discuss differentiated models of care for transgender people with examples from Kenya and South Africa on experiences in implementing community-based models aimed at providing optimal health care services for the community in sub-Saharan Africa. A moderated discussion following the presentations allowed participants to voice their opinions and provide recommendations on tailoring services for this key population group.
——
Following the meeting, CQUIN and SSLN will continue to foster the exchange of best practices, resources, and lessons learned with regards to optimizing the coverage and quality of HIV services for key population groups. Building on the country action plans submitted following the August meeting, CQUIN will launch a community of practice focused on differentiated key population services. The CQUIN webinar on Tuesday, October 5, 2021, at 8 am EST will explore DSD for people in prison, and CQUIN’s 5th Annual Meeting in November will include multiple parallel sessions on DSD for KP. Register here.