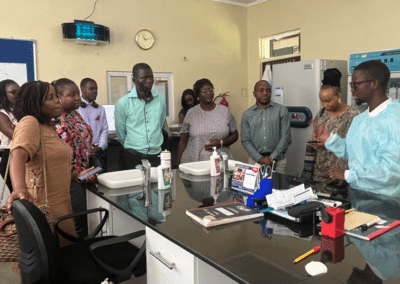
Gang Sun, MD, is the UNAIDS Testing and Treatment lead and a CQUIN Advisory Group member. Dr. Sun participated in the March Differentiated Testing Across the HIV Cascade meeting in Nairobi, where he was a panelist in a plenary discussion on the latest strategies for differentiated HIV testing services (dHTS) and a moderator for a plenary session on community involvement in dHTS. After the meeting, he sat down to chat with us and shared some insights on the importance of CQUIN’s support for network partner countries.
You moderated the community involvement in dHTS session, where two community organization leaders shared interesting case studies on their work linking men who have sex with men to HIV testing, prevention, and treatment services. What were some of the key messages of that panel?
That session focused on the role of the community in promoting differentiated service delivery, particularly for differentiated testing and linkage to services. The panelists were excellent. These are two community leaders with a wealth of experience, heading projects in collaboration with key populations and men who have sex with men. In a way, what they have done is offer services for the people by the people who need the services the most in a very friendly way. This helps many people to know their HIV status in time and immediately get linkage to sexual, reproductive, HIV, NCD services, and more. They also showed how things could work in Kenya, where the legal environment is not perfect. When these examples are presented to more partners, best practices can be replicated and scaled. Without good services in scale, we won’t get the impact we want, which echoes that community partners can be a very significant asset in implementing health systems.
Thinking about the CQUIN meeting, which issues were of high interest and created opportunities for learning?
This is my second time attending a CQUIN meeting, and I’m privileged to observe how well countries are managing their programs with strong technical support and guidance from ICAP and other key partners like the WHO, CHAI, ITPC, and IAS. The value of community and its role has been appreciated through all the different sessions of this meeting, and I really value CQUIN meetings for prioritizing this. At the end of the day, we are all working together for the communities, and there shouldn’t be anything for them without them. I also recall the GIPA [greater involvement of people living with HIV/AIDS] principle, which is the greater involvement of people from all angles, from planning to research, monitoring, and evaluation, so the recipients of care can be the designers as well as providers of services. We’ve seen here that, in many cases, they can do great work. I hope all the participating countries will institutionalize community involvement in many of their programs. Some of these discussions have been reflected in the country feedback, where I can see what has been learned here can immediately translate into the Global Fund and COP 23 funding request as part of funding negotiations and discussions.
What do you think are the top priorities for differentiated HIV testing in 2023?
I do not want to preempt what the great minds in the meeting hall generated, but just from my observations and what I’ve learned, countries could probably fine-tune a monitoring system that reflects the work on scaling up testing services. On the prevention front, it is critical to think of linking services through status-neutral testing, but I want to add a point. We don’t have to reinvent all the wheels. I am happy to see that in presentations, countries are referring to systems already in place, for instance, the UNAIDS Global Prevention Coalition, which includes the 28 countries with most of the new HIV infections in the world. The Coalition Road Map for 2025 prioritizes five prevention pillars. I have seen the five prevention pillars referred to at the meeting, and I also know that work plans are being produced in those countries as part of the Global Prevention Coalition movement, so that is already a well-thought-of package. What we can do here is to open the doors of status-neutral testing. To set up linkages for that, not to reinvent all the indicators which are already there. Similarly, all countries identified pediatric care and testing are also lagging compared to the general population, and that is an area where we can tap into ongoing initiatives, including the Global Alliance to end AIDS in Children by 2030.
How do you think the CQUIN network can help to advance the coverage and quality of HIV testing and linkage services?
It would be very helpful for CQUIN to link up with those initiatives I have mentioned. That is what I see as coming out of this very good meeting. I also want to praise CQUIN for the many good tools established. For example, the capability maturity models play a key role in giving countries direction to self-assess their gaps and needed areas of support.