Optimizing Quality in Person-Centered HIV Care: Pilot Implementation of the Key Population-Friendly Service Quality Management Toolkit
Despite significant progress toward the UNAIDS 95-95-95 goals, key populations—such as men who have sex with men, sex workers, transgender individuals, people who use drugs, and prisoners—continue to face stigma, discrimination, and systemic barriers to accessing HIV services. To bridge this gap, the Key Population, Quality Management and Monitoring and Evaluation Communities of Practice developed a Key Population-Friendly Services Quality Management Toolkit as an innovative solution to ensure equitable, accessible, and high-quality HIV care in public health facilities. The toolkit defines quality standards for KP friendly services at government health facilities with an assessment questionnaire that supports national health care systems in delivering truly inclusive services.
Why This Toolkit Matters
The KP-Friendly Service Quality Management Toolkit embeds human rights-based and person-centered care into national health systems. Regular use of this assessment could drive sustainable improvements in key population-friendly services across six key dimensions:
- Equitable: Policies must ensure the right to health care for all, regardless of key population status.
- Accessible: Facilities work to remove common barriers faced by key populations when accessing services.
- Acceptable: Robust mechanisms must be in place to prevent and address stigma, abuse, and harassment, while ensuring confidentiality and safety for key populations accessing services.
- Appropriate: Routine and tailored services, such as harm reduction for people who use drugs, should be available and integrated into national HIV programs.
- Effective: Facilities must collect and analyze service utilization data disaggregated by key population status to monitor quality and drive continuous improvement.
- Accountable: Communities must be empowered and equipped to advocate for quality services, with direct involvement in service design, service provision, and monitoring efforts.
By operationalizing this toolkit, Ministries of Health can work to reduce stigma and discrimination in public health care settings, integrate key population-specific health needs into routine services, enhance community engagement, and strengthen monitoring and accountability mechanisms.
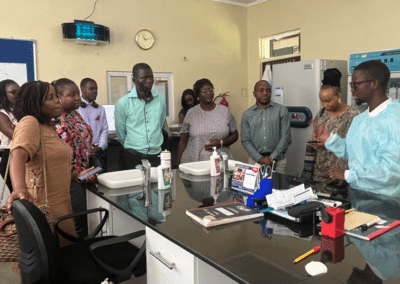
Pilot Testing for Local Adaptation
To ensure the toolkit’s effectiveness, the quality management team have a structured pilot testing phase planned to refine its implementation before broader rollout. Ministries of Health, health management teams, and implementing partners will assess the toolkit at selected government health facilities, with a focus on:
- Identifying the toolkit’s strengths and areas for improvement
- Ensuring alignment with national health policies and standards
- Providing essential baseline data for targeted interventions
- Supporting the development of a quality monitoring framework aligned with person centered services, regional, and global HIV program sustainability goals.
CQUIN member countries are invited to volunteer to participate in the pilot phase of the Toolkit, that will shape the future of HIV service delivery for key populations. Participating countries will receive technical support and will play a critical role in refining and adapting the toolkit to ensure its sustainability and impact.
To express interest or learn more, please contact:
Cassia Wells – caw2208@cumc.columbia.edu
Gillian Dougherty – gd2410@cumc.columbia.edu
Onyekachi Ukaejiofo – ou2122@cumc.columbia.edu
Together, we can make quality, person-centered HIV services a reality for all key populations.