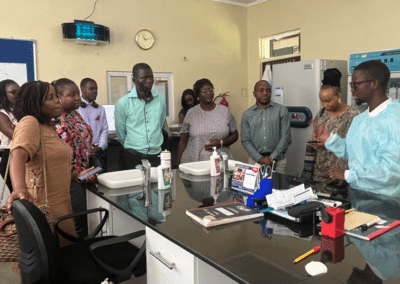
Setting targets for the scale-up of integrated services was top of mind for most participants at the CQUIN Integration Meeting. Here are a few participant views on what countries need to scale up non-HIV services into DSD Programs.

Helen Bygrave, Consultant, IASWe know our recipients of care are getting older. We know they are going to present with noncommunicable diseases like hypertension. In fact, we that more people with HIV are dying of hypertension than are of opportunistic infections. So, we need to look at the guidelines and then the medicines. How do we prescribe the medication so that recipients of care can pick up their antiretroviral therapy every six months but also not have to come to the clinic and get in a queue to get their blood pressure medicines? Because we know there are limitations, we need to work together in the clinic with our pharmacy colleagues to make sure patients are getting their hypertension medicine easily in an easy way whilst aligning clinical visits. So, I would start by having very clear guidance that enables scale-up and every clinic in your country to do the same thing, use the same algorithm, and have the same frequency of visits. Once you’ve got your clinical guidelines and you’ve decided what blood pressure treatments you need, then we can start negotiating about buying those medicines and the price of those medicines.
I would love to hear some commitments from funders, policymakers, and programmers on how to scale up integration at that high level. This is because many times when we talk about integration, and we get into countries, you realize that a lot of integration is discussed from the service delivery point of view, and yet for that to happen, integration needs to be thought of from a policy level. How are we integrating our policies and funding mechanisms? And how do we think of programming at that level that is not disintegrated and is not donor-driven but recognizes that there is a need for people at the policy level to sit at the same table to come up with common programs and funding mechanisms that are going to address integration? So, my call to action from this meeting will be strong recognition and appreciation that integration can only work if people at the policy level have committed to it. Lastly, and not least, we need to have a way to call on our governments to be part of this agenda, particularly making sure that domestic financing is made real. We can talk about donors and external partners, but they are not going to do much. Countries must invest in systems and human resources for health.
Lilian Mworeko, Executive Director, International Community of Women Living with HIV in East Africa, ICWEA


I would say the most significant barrier to HIV/HTN integration is supply chain management – the availability of medicines. However, a second one worthy of mention is the lack of information systems to track outcomes or monitor your implementation. What we see is that there’s a stark contrast between the supply chain system for HIV medicines and the supply chain system for hypertensive medication. While in HIV, you have a reliable system – the medicines are there, they are dispensed at no cost to the recipient of care, and you have robust systems to monitor and track consumption, distribution, and utilization of commodities – it’s not the same for NCDs. When it comes to NCD treatment, especially in Africa, there are a lot of medicines, but there are doubts about the quality of those medicines. Then, there are the frequent stock-outs of NCD medicines at facilities. The other thing is that NCD medicines come at a cost, and these are just some of the challenges. Of course, it requires a lot of advocacy for governments to commit to funding the procurement of medication. However, some of the general solutions we propose are to start by aggregating demand first. You need to create demand. To create demand for these hypertension medicines, you need to develop a simple treatment protocol because, by the time you develop a simple treatment protocol, the entire country has pivoted to start using the treatment protocol. It means you will generate volumes for those medications on the treatment protocol and then use that as leverage so the government can negotiate lower prices.
Kufor Osi, Senior Technical Advisor (Hypertension), Resolve to Save Lives