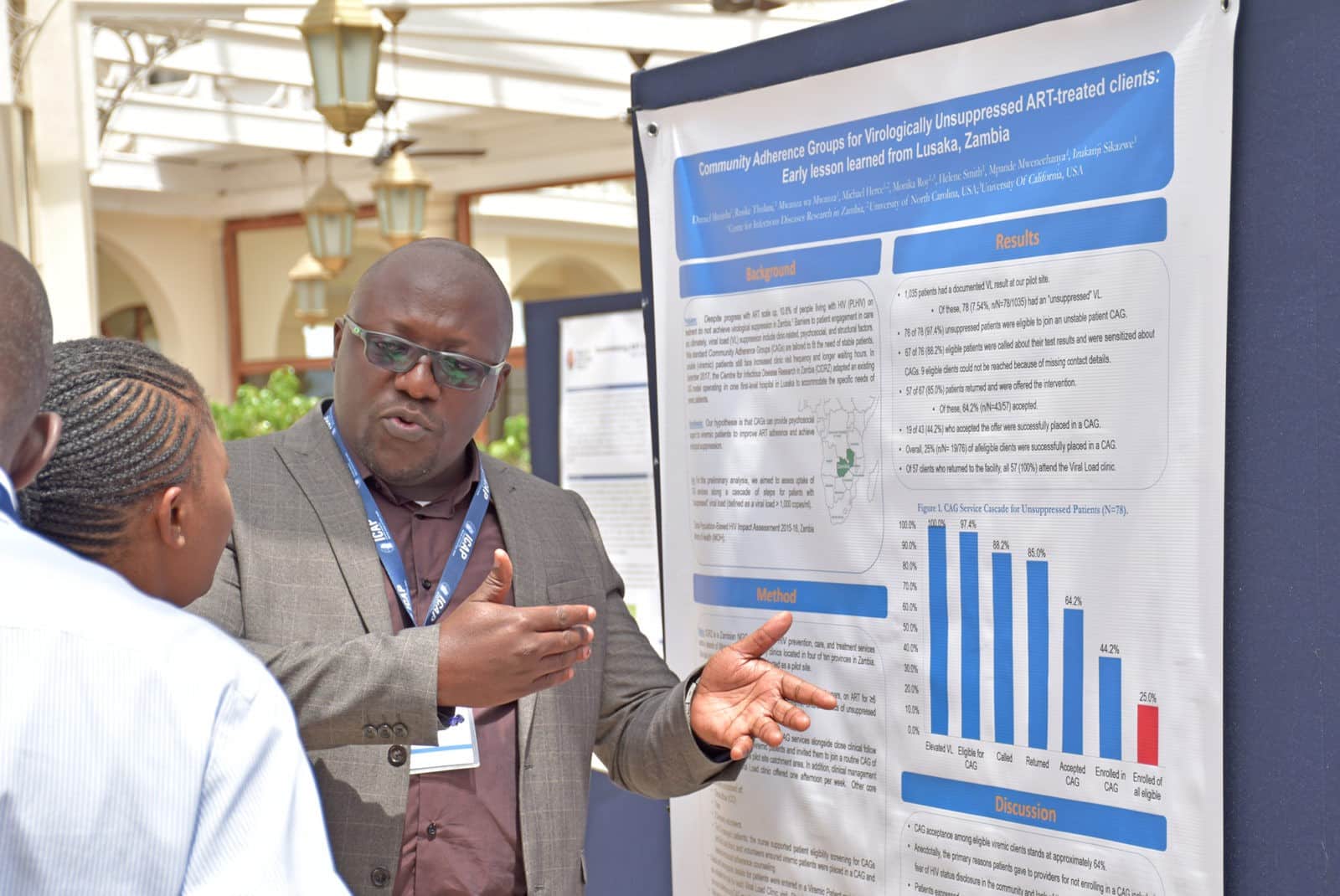
Dr. Mwamba is the Lusaka ART Coordinator at the Centre for Infectious Disease Research in Zambia (CIDRZ), and an active member of the CQUIN Network. Last summer, he shared his insights on DSD, including the challenges of achieving quality care with limited resources, and the future of HIV care and treatment.
How does your work relate to differentiated service delivery (DSD)?
I oversee all antiretroviral therapy (ART) clinics that the Center for Infectious Disease Research in Zambia (CIDRZ) supports in Lusaka province. It’s my job to ensure we provide quality care to all HIV patients across 112 health centers, but this is not always easy when you have limited number of health care providers and an increasing number on patients. We have been implementing DSD models to help alleviate the crowding in our clinics and reduce the burden on our systems for two years now. It works to the satisfaction of both patients and health care providers.
Why is DSD important for Zambia?
Zambia has a high HIV burden. As a developing country, the cost implication of running an ART program can significantly impact the country resource allocation. Besides being a patient-centered approach to deliver ART services, DSD is also a cost-effective way of providing quality care. Differentiated service delivery promotes task shifting from health care providers to trained community lay workers, and certain DSD models shift the service from health facility to the community. This results in immediate patient satisfaction. At the national level, it’s a cost saving strategy for places with limited health care providers that also helps maintain the standard of care.
What do you hope to see concerning DSD in the next few years?
It will be nice to have as many DSD models as possible to suit each patient preference and scale them up to all eligible patients in Zambia. Beyond HIV, we should be able to integrate non-communicable diseases and other chronic illnesses into ART, so we can provide an integrated chronic illness package through DSD.
What are some of your unanswered questions about DSD?
We know what we want to achieve for stable patients. For patients at high risk of disease progression, it’s less clear. As a clinician, my main priority is not only the large group of patients that are doing well—it’s also the smaller group of patients who are not doing well. Differentiated services for stable patients helps decongest heath facilities and allows clinicians to spend more time on those patients who may need more attention. There’s a lot of work that needs to be done to design models tailored to the needs of unstable patients – perhaps something like a community package.
At CIDRZ, we are adapting an existing community adherence group (CAG) model to accommodate patients with raised viral load. Our hypothesis is that stable patients will provide psychosocial support to the viremic patients and ultimately help them improve adherence to medication and achieve virologic suppression. I hope we can share lessons learned at upcoming CQUIN meetings.
What are some challenges you’ve faced in this work?
The biggest challenge we are facing is the high level of attrition and number of patients who refuse to start or decide to stop their medication. This is across all ages, sexes, level of education, and socio-economic status. When I was reviewing a young woman’s patient chart recently, I noticed she had a very high viral load. Mind you, she was already on second-line ART. I looked into it and found out that this patient is one of our best adolescent peer educator at CIDRZ. She counsels and gives support to HIV patients every day.
After speaking to her, I learned that she was born with HIV and raised by her late mother, who was also HIV positive and on treatment before she passed. After she lost her mother, she fell into a deep depression. She said to me, ‘What’s the point of taking my ARVs?’ ‘My Mom took them, and she’s no longer here.’
Her mother was her treatment support. When she died, she stopped taking treatment, but still, encouraged her clients to take their medication. We identified an elderly female psychosocial counsellor who was very close to this young girl and assigned her to be her treatment supporter. I am proud to say that the girl has since confirmed that she is now taking her treatment consistently. She is so happy to have someone looking over her.
What I learned from this experience is that every patient has a story to tell. Patients do not stop treatment for no reason. If we take time to listen to each patient and provide the appropriate intervention tailored to each case, we will reduce attrition.
How do you see the CQUIN network helping you and your colleagues scale up DSD in Zambia?
Currently in our national ART guidelines there is a mention of DSD, but there has been no implementation at the national level. Right now, different NGOs and partners are implementing various DSD models, but there is no cohesion. With the support of CQUIN and collaboration with the Zambia Ministry of Health, we are working to develop standard national DSD guidelines, and ultimately work toward implementation and large coverage.
This interview is part of the series: Perspectives on differentiated service delivery, exploring expert views and insights into the importance of DSD in sub-Saharan Africa, and the unique challenges they face in advancing services for people living with HIV. For more updates on this series, and other network activities, sign up for our newsletter monthly newsletter.