The Acting Executive Director of the Zimbabwe National Network of People Living with HIV speaks about her role ensuring the needs of people living with HIV are met; unanswered questions for key and priority populations; and CQUIN’s role in strengthening partnerships.
How does your work relate to differentiated service delivery (DSD)?
The Zimbabwe National Network of People Living with HIV (ZNNP+) is a membership organization of People Living with HIV (PLHIV). We advocate for services for these individuals. My role is ensuring that the needs of PLHIV are being addressed by the government and its partners, including development organizations. We also ensure that PLHIV can access the services they need and that their rights are respected when doing so. We develop programs that speak to their needs.
Why is DSD important in Zimbabwe?
People are different and so are their needs. We had a one-size-fits-all approach to service delivery until recently, which means people go to the health facility, pick up their medication, and go home. Psychosocial support was done primarily at the community level. We realized PLHIV were going to health facilities and spending a lot of time there when they are not necessarily sick.
The first DSD approach we rolled out was community ART refill groups (CARGs). This gave people the opportunity to get drug refills or pickups done by someone else. We were noticing that not everyone that wanted to be part of a group. Some still feel they need to pick their drugs up on their own, and when they do, they don’t want to spend a lot of time at the health center. They prefer a fast track refill, or for someone from the facility to bring drugs to the community so they can get them closer to home.
We don’t all have access to the same information. The ‘how’ and the ‘why’ often go unanswered at the community- and service-provider levels.”
What do you hope to see with regard to DSD in the next few years?
In Zimbabwe, there has been a lot of investment in creating simple DSD models; this includes CARGs. In some institutions, there are fast-track drug pickups that are happening. We are also seeing small-scale, family-centered approaches where one family member will pick up medicine for their relatives.
We want all of these service delivery approaches to be available to the community. We may start by looking at popularizing these service approaches so that people know that there are options. We also want to inform providers that these service models can be offered to communities.
What are some of your unanswered questions about DSD?
We appreciate the role of the health center to put the client closer to the service provider. My unanswered question is: What we do for high-risk or unstable clients? Should they be spending a lot of time at the health facility? Should we come up with an intervention that speaks to them? There is also the issue of key and priority populations. We know that it may be uncomfortable for them to be part of a CARG, but we also know that if they are empowered enough, they will be part of these groups.
We’re still unsure of what the best model is for them. Should we open clinics in areas where they can come during the night? In Zimbabwe, we have issues with miners, who spend most of their days in informal settlements trying to make a living. These individuals cannot spend the entire day in queues, so what is the best time for them to get a refill? Unfortunately, the default rate is high among this population because they do not have time to go to the facility and they prioritize making a living over getting a drug refill or pickup.
What are some challenges or barriers you have faced?
Issues of capacity and knowledge among community members and service providers. There are many unanswered questions within the health services delivery system. At times, there is a general lack of understanding, and questions are asked from an uninformed positon. Most people informed about DSD are probably at a higher level, perhaps provincial, but most of this work is done at the facility level and we don’t all have access to the same information. There are standard operating procedures, but the ‘how’ and the ‘why’ often go unanswered at the community- and service-provider levels.
How do you see the CQUIN network helping you and your colleagues to scale up DSD in Zimbabwe?
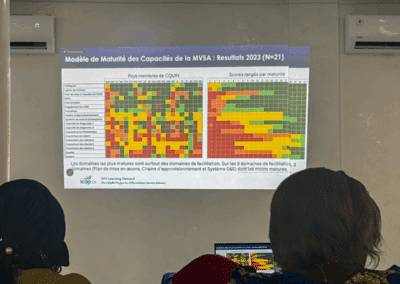
At the country level, we are a stronger team. We now have a platform where we can exchange notes, and conduct peer review of country level work. Now implementing partners and the ministry of health all have a stronger relationship that comes with a shared objective of rolling out DSD models.
There is a higher level of experience sharing. There’s a lot of information, and we are already thinking of ways we can replicate the same approaches and address our common challenges. There’s a lot of research that is currently going on in different countries, and it’s an opportunity to learn from the body of knowledge that currently exists.
This interview is part of the series: Perspectives on Differentiated Service Delivery, exploring expert views and insights into the importance of DSD in sub-Saharan Africa, and the unique challenges they face in advancing services for people living with HIV. For more updates on this series, and other network activities, sign up for our monthly newsletter.