From November 4-8, 2024, a delegation from Zimbabwe, including representatives from the Ministry of Health and the Zimbabwe National Network of People Living with HIV (ZNNP+), visited Malawi for a CQUIN-supported Country-to-Country (C2C) learning exchange. The delegation traveled to Lilongwe, the capital of Malawi, to explore differentiated service delivery (DSD) models and share knowledge on best practices for ensuring that people living with HIV (PLHIV) remain in care and to re-engage those who have interrupted treatment.
This exchange was particularly timely as Zimbabwe is scaling up its own DSD efforts, focusing on re-engagement and retention strategies. The visit covered the full cascade of care — from identifying individuals at risk of disengagement, to tracing and re-engaging those who have interrupted treatment, and ultimately improving retention. A central focus was Malawi’s innovative “Welcome Back Package”—a strategy designed to ensure that individuals who return to care after an interruption are supported in their reintegration journey.
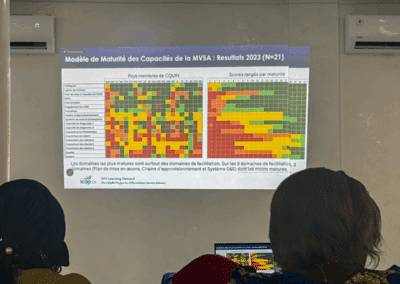
The learning visit delegation during a presentation session.
The Zimbabwean delegation visited several key health care facilities to observe these strategies in action and gain insights into the resources, processes, and tools involved in re-engagement efforts. Each visit provided valuable information on how various models of care were applied at both the community and facility levels.
The first site visited was Area 25 Health Centre, which had a total ART population of 23,150 as of September 2024. Supported by a PEPFAR/USAID implementing partner, Partners in Hope, the center has integrated a cyclical cascade approach to managing HIV care. During the visit, the delegation observed the Health Management Information System (HMIS) in action. This system generates a line list from the electronic medical record (EMR) to pre-call patients due for appointments. The EMR automatically categorizes patients based on their level of disengagement — missed appointments (within 7 days), defaulters (7-28 days), and those lost to follow-up (more than 28 days).
The team also examined data systems used to track patients, including a phone call logbook documenting tracing efforts by adherence counselors and health surveillance assistants (HSAs), as well as a case management register for follow-up. A critical part of this process is the “Welcome Back” service, which includes counseling and support to ensure that returning patients feel welcomed and motivated to continue their treatment.
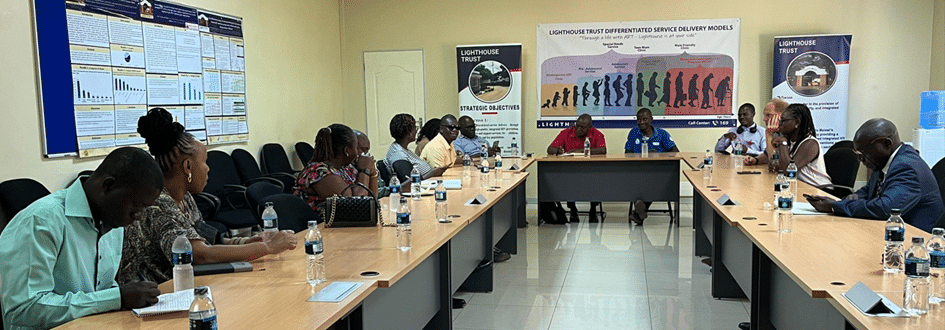
The second site visited was LightHouse, a PEPFAR/CDC-funded implementing partner at Kamuzu Central Hospital. Known for its proactive approach to client tracing and re-engagement, this facility utilizes the 4D strategy — Deflate, Discuss, Direct, and Decorate — when a patient disengages from treatment. Once identified as disengaged, the patient is traced, re-engaged in treatment, assigned a case manager (via a buddy system), and followed up for up to 12 months. This patient-centered model helps patients feel supported and increases retention.
The final site visited was Kayembe Health Centre, a non-partner supported facility. Despite having fewer resources, this center successfully implements many DSD strategies, including flexible clinic hours and phone reminders for patients due for appointments. This demonstrated how DSD initiatives can be sustained even without direct partner support.
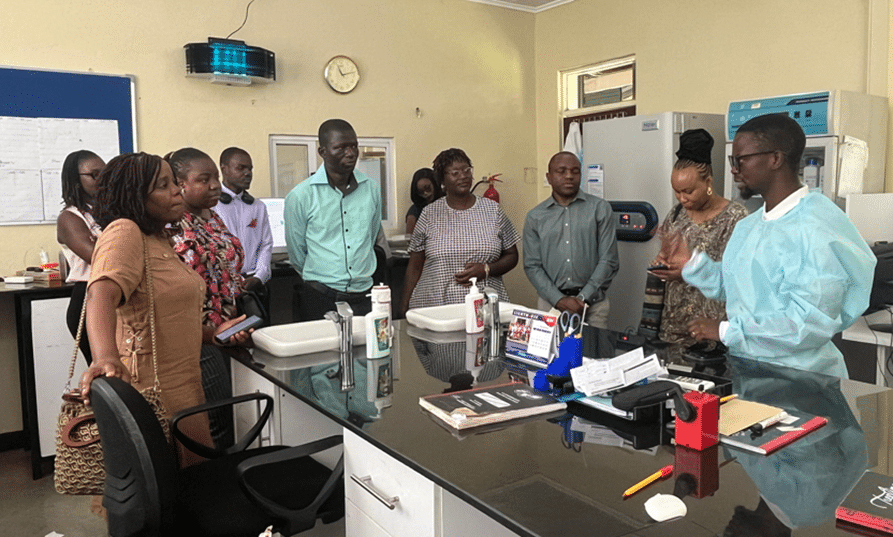
The Zimbabwe team touring the LightHouse Laboratory, gaining insights into effective care strategies.
Delegates during a site visit, gaining insights into effective care strategies. Zimbabwe plans to develop a similar “Welcome Back Package” for individuals who re-engage in HIV care after an interruption. This will include enhanced support for newly initiated patients and strengthened retention efforts for those returning to care. New ideas emerged during the visit, including opening men’s clinics, establishing high viral load clinics, providing follow-up for up to 12 months, and using phone call or SMS reminders to ensure patients attend their appointments.
Another key takeaway was the importance of contextually adapting Malawi’s “Back to Care” program — particularly the buddy system and community-based counseling — to suit Zimbabwe’s unique needs. The team emphasized the need to create non-judgmental guidance for patients returning to care to ensure a welcoming environment for all. The visit also highlighted the vital role of national health systems in supporting re-engagement efforts, especially in non-partner supported facilities.