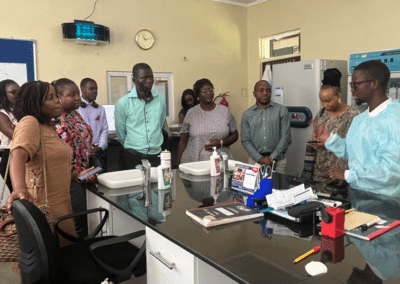
Mbabane, Swaziland – At a CQUIN experience-sharing meeting hosted by ICAP Swaziland, Dr. Maureen Syowai from ICAP in Kenya greeted the Swazi and Zimbabwean audience with a warm “Sanibonani”. Dr. Syowai skillfully conveyed her country’s experiences with implementation and scale-up of differentiated service delivery (DSD) to an audience of about 30 participants from ICAP Swaziland, the Swaziland National AIDS Program (SNAP), and the Zimbabwe Ministry of Health and Child Care (MoHCC). Her presentation quickly blossomed into a lively dialogue with the audience, sparking new ideas for systematic and rapid roll-out of DSD.
Dr. Clorata Gwanzura, a Medical Officer with the Zimbabwe MoHCC, applauded Kenya’s ability to create demand for DSD models. “In our approach we haven’t stressed demand creation and the impact it can have,” she said. “That’s one aspect that we have to look into when we are doing our training and sensitizations – to really reinforce implementation of these models.”
“The concept of differentiated service delivery is still new, so many countries are still figuring out a process of defining models for different groups in care,” said Dr. Ruben Sahabo, director of ICAP in Swaziland and the lead organizer of the meeting. “Maureen’s talk was very important, because she was able to share how Kenya went through the process of designing models and developing tools, how the models were implemented in MoH facilities. Swaziland shares a lot of the same challenges as Kenya, so we can learn from their experience. This south-to-south exchange is exactly the kind of forum for sharing knowledge, lessons learned, and allowing opportunities for people to ask questions and generate new ideas.”
Drawing comparisons between Kenya and Swaziland, Dr. Syowai highlighted lessons learned at both the national and provincial level in Kenya, and how their experiences could be applied in Swaziland, a country with a smaller population and higher HIV prevalence. The county of Siaya in southwestern Kenya, for example, has a similar population size (1 million) and HIV prevalence (24 percent) to Swaziland’s 1.1 million and 23 percent prevalence rate. Dr. Syowai showed data highlighting the success of enrolling stable patients in fast-track refills and community ART groups in Siaya, along with other models.
Dr. Nomthandazo Lukhele, National ART Coordinator at SNAP, urged the implementers in the audience working in Swaziland to focus on standard operating protocols (SOPs). She noted that Swaziland had made great strides in creating SOPs for successful DSD models in-country, but was careful to note that continued progress will require bringing in more monitoring and evaluation (M&E) registers for clubs and community ART groups.

Dr. Nomthandazo Lukhele
Dr. Syowai explained that country leadership and community ownership of scale-up and national policies and guidelines for M&E were key enablers to the success of DSD in Kenya. The audience pointed to gaps in M&E tools that persist in Swaziland, one of the issues that the CQUIN network is helping to solve via its M&E consultation in Swaziland. In the days leading up to the meeting, Dr. Bill Reidy, an epidemiologist at ICAP and a clinical advisor to CQUIN, accompanied Dr. Syowai on a technical assistance visit on M&E of DSD in Swaziland. Lessons learned will inform CQUIN’s new Community of Practice on M&E of DSD.
This story is part of a series focused on the evolution of the CQUIN network, and countries’ progress in improving differentiated service delivery. To follow this story and others, sign up for the network’s monthly newsletter.