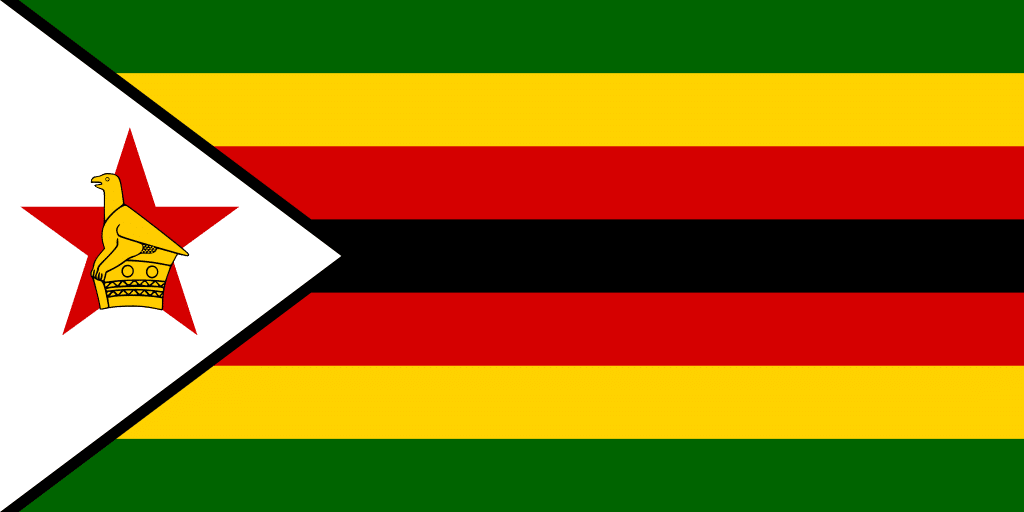
 Zimbabwe
Zimbabwe
Differentiated Service Delivery in Zimbabwe
Facility-Level
Coverage
%
% In Less-Intensive
Differentiated Treatment Models
%
Multi-month ART Dispensing
%
DART Model
Diversity
Differentiated Service Delivery Implementation in Zimbabwe
Zimbabwe has been a member of CQUIN since the network first launched in 2017. Differentiated service delivery (DSD) policies in Zimbabwe are supported by the national government’s HIV and ART guidelines and include operational and service delivery procedures to prioritize recipients of care doing well on antiretroviral (ART) medication and strengthen supply chain management and community health systems.
Zimbabwe was an early adopter of decentralization of care and task-shifting and has seen successes in retention through implementing DSD with adolescent and peer-led approaches. Recipients of care have played an integral role in shaping DSD programs through participation in community groups such as the Meaningful Involvement of People Living with HIV and AIDS Forum (MIPA), which works with Zimbabwe’s Ministry of Health and Child Care (MOHCC) to discuss programmatic updates and issues affecting people living with HIV.
Currently, Zimbabwe offers six main less-intensive DSD treatment models, including:
- Two Facility-Based Individual Models: three-month multi-month scripting; and fast track.
- One Facility-Based Group Model: facility club refill model, which includes the teen club model.
- One Community-Based Individual Model: community outreach model.
- Two Community-Based Group Models: community ART refill groups; and family ART refill groups.
Building monitoring and evaluation (M&E) capacity is a priority for Zimbabwe’s DSD program and the country has made progress in this area. In 2018, the Zimbabwe MOHCC developed a DSD-specific M&E plan with support from CQUIN. CQUIN has also supported Zimbabwe to conduct two DSD Performance Reviews – ad hoc data collection exercises to review DSD coverage and quality at selected facilities. In addition, after a CQUIN-supported south-to-south learning exchange to observe Eswatini’s client management system, Zimbabwe deployed a new electronic patient management system in case-based surveillance pilot districts. This new system shows great potential to improve M&E by allowing staff at health facilities to enter recipient of care data collected from booklets into the digital system—an innovation that will lead to a more timely and accurate understanding of DSD coverage.
Other priority areas that Zimbabwe’s DSD program seeks to improve include the development of quality standards, and the need for DSD models that address highly mobile populations in urban areas. Though Zimbabwe has seen success in community-based ART refill groups, male engagement continues to be low. To understand this challenge, CQUIN and MOHCC partnered in a study to explore the barriers and facilitators of male engagement in community ART refill groups (CARGs). CQUIN and MOHCC have also partnered on a study of the feasibility and acceptability of delivering tuberculosis preventive treatment (TPT) in the CARG setting.
As Zimbabwe’s DSD program continues to mature, participation in CQUIN communities of practice—including those on M&E, quality and quality improvement, and people at high risk of disease progression—are key to gaining new insight and co-creating tools to enhance national DSD implementation.
Resources
Taking Differentiated Service Delivery to Scale in Zimbabwe
Mantell et al Engaging Men JIAS 2019
Engaging men in HIV Programmes: a qualitative study of male engagement in community‐based antiretroviral refill groups in Zimbabwe

Visit ICAP's Website for a broader portfolio of work in CQUIN network countries.