“For me, treatment in the HIV clinic is just getting my antiretrovirals. For my asthma, high blood pressure, and my enlarged heart condition, I go to a private facility every four months or when the need arises for treatment and medication,” said Patricia Asero, a recipient of care living with HIV and hypertension. “I feared talking about family planning; no one in my clinic introduced that topic,” said Lillian Mworeko, another recipient of care, thinking back to when she needed family planning services.
When HIV programs started in Africa, ministries of health established National AIDS Control Programs (NACPs) to reach and treat people living with HIV to reduce the burden of the disease rapidly and efficiently. With established NACPs reaching their set targets of reducing HIV with effective treatment programs, including differentiated service delivery – a person-centered approach to HIV prevention, testing, and treatment, many studies show that, in general, recipients of care are living longer. However, because HIV programs were primarily established and funded to treat HIV, recipients of care who live with HIV and other health conditions and needs sometimes find themselves lacking comprehensive primary health care.
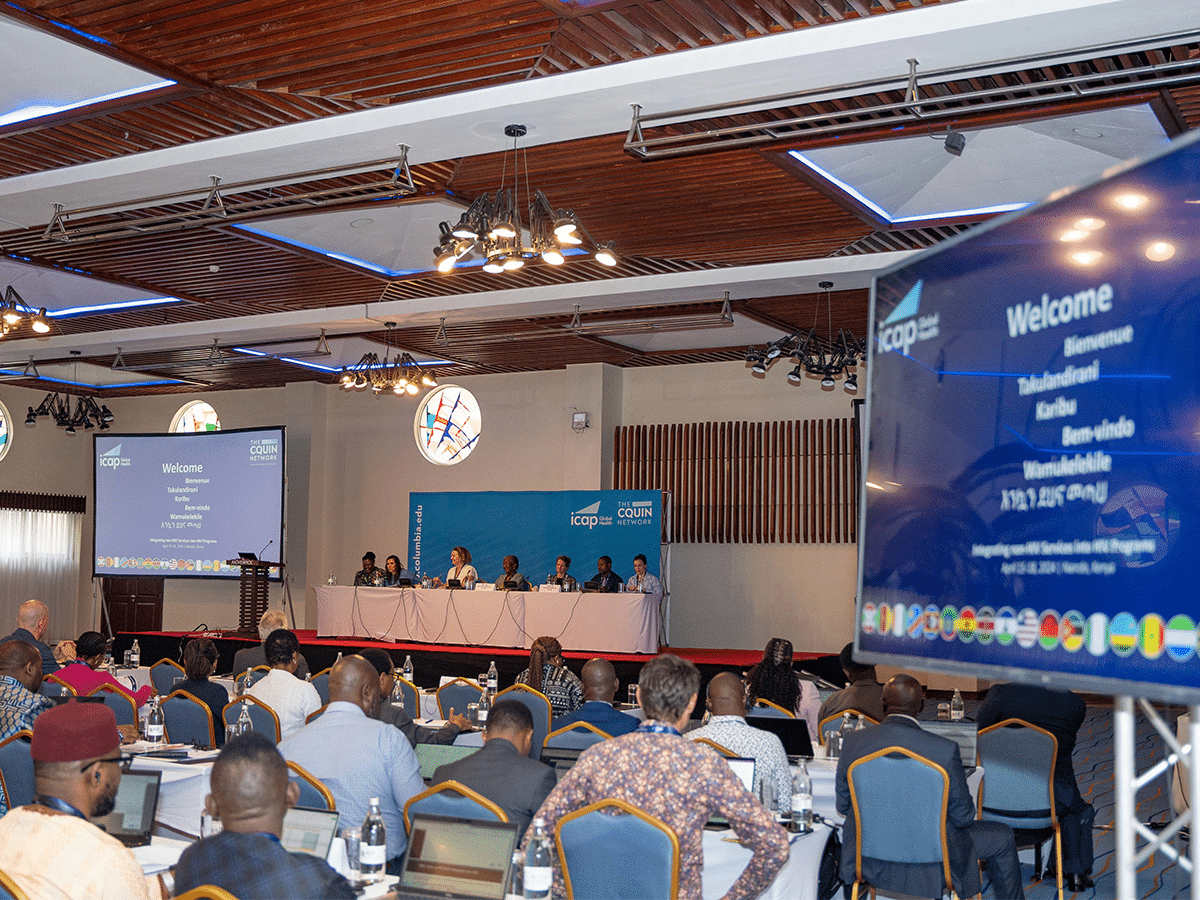
These health care gaps for recipients of care are what prompted CQUIN’s first-ever Integrating Non-HIV Services into HIV Programs Meeting, as part of the network’s focus on shaping models of HIV treatment that meet the specific needs of people established on HIV treatment.
“Integration is critical for recipients of care,” said Maureen Syowai, MBChB, MSc, CQUIN deputy director for technical at the meeting. “Health system leaders need to ensure people receive HIV and non-HIV services that will complement their full range of health care needs.”
From April 15 to 18, 2024, in Nairobi, Kenya, CQUIN convened approximately 240 participants, including Ministry of Health representatives from all 21 CQUIN network member countries, recipients of care organizations, implementing partners, and global stakeholders to share best practices, country case studies, and discuss common challenges to make recommendations on integrating non-HIV services, including family planning (FP), and hypertension (HTN) services into differentiated service delivery (DSD) programs.

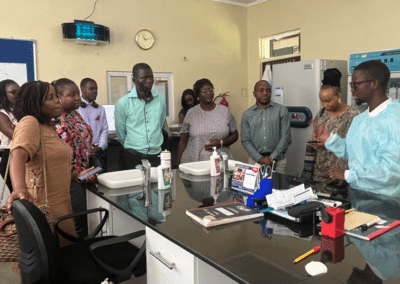
Some meeting participants at a tools presentation by a team from Malawi
Participants also discussed the granular “who/where/how /when” building blocks of program design and key issues, including coordination between Ministry of Health departments, donors, and implementing partners and ensuring that national policies, guidelines, training curricula, procurement and stock management systems, and monitoring and evaluation systems are optimized for integrated services at the point of care.
“We wanted to orient countries and make a solid case for why integration is important, and as a learning network, we want to build on lessons from countries in the network to lay the foundation of how we can start to integrate and scale up programs to meet the needs of recipients of care,” said Peter Preko, MBChB, MPH, CQUIN principal investigator and project director.
Highlights – Progress Challenges and Opportunities for Family Planning and HIV Integration
“The integration of interventions not only promotes person-centered care but also reduces incidence, morbidity, and mortality from infectious disease and strengthens disease monitoring and program planning,” said Morkor Newman, MBChB, MPH, medical officer EMTCT with the WHO in a plenary session on family planning and HIV services integration. In the session, presenters and panelists talked about the limitations and challenges to FP/HIV integration, including current guidelines and recommendations for integration from the WHO, issues with the supply chain of FP commodities, and case studies on how to integrate FP services into DSD programs. Countries also provided case studies on FP/HIV integration models they are implementing.
Progress Challenges and Opportunities for the Integration of HIV and Hypertensive Services
According to studies, an estimated six million people living with HIV in sub-Saharan Africa also have hypertension. In this session, panelists and speakers talked about the importance of prioritizing hypertension treatment for people living with HIV, as the disease affects 1 in 3 adults worldwide and is the leading cause of strokes, heart attack, and heart failure in adults. A presentation by Kufor Osi from Resolve to Save Lives addressed the burden of hypertension in PLHIV and RSTL’s approach to ensuring effective hypertensive care for people living with HIV in five case-study countries. Other presenters discussed the importance of hypertension control programs, differentiated service delivery for hypertension, and how country programs could set targets to procure hypertension medication.
Meeting discussions also delved into monitoring and evaluating integrated programs and questions on how best to lead program integration at the ministry level. Further discussion and learning exchange took place with a presentation of tools that reflect the integration of non-HIV services into DSD programs and at poster sessions, where participants presented examples of integration at various health care system levels.

Monitoring and Evaluation (M&E) officers from various country teams at an M&E pre-meeting
Following meeting discussions, country teams discussed lessons learned and best practices from the meeting to develop action plans that would foster commitments to improving HTN/HIV and FP/HIV integration at a national level, which the ICAP CQUIN technical team will follow up on.
All the meeting content, including slide presentations, shared tools, and posters, are available on the CQUIN website.