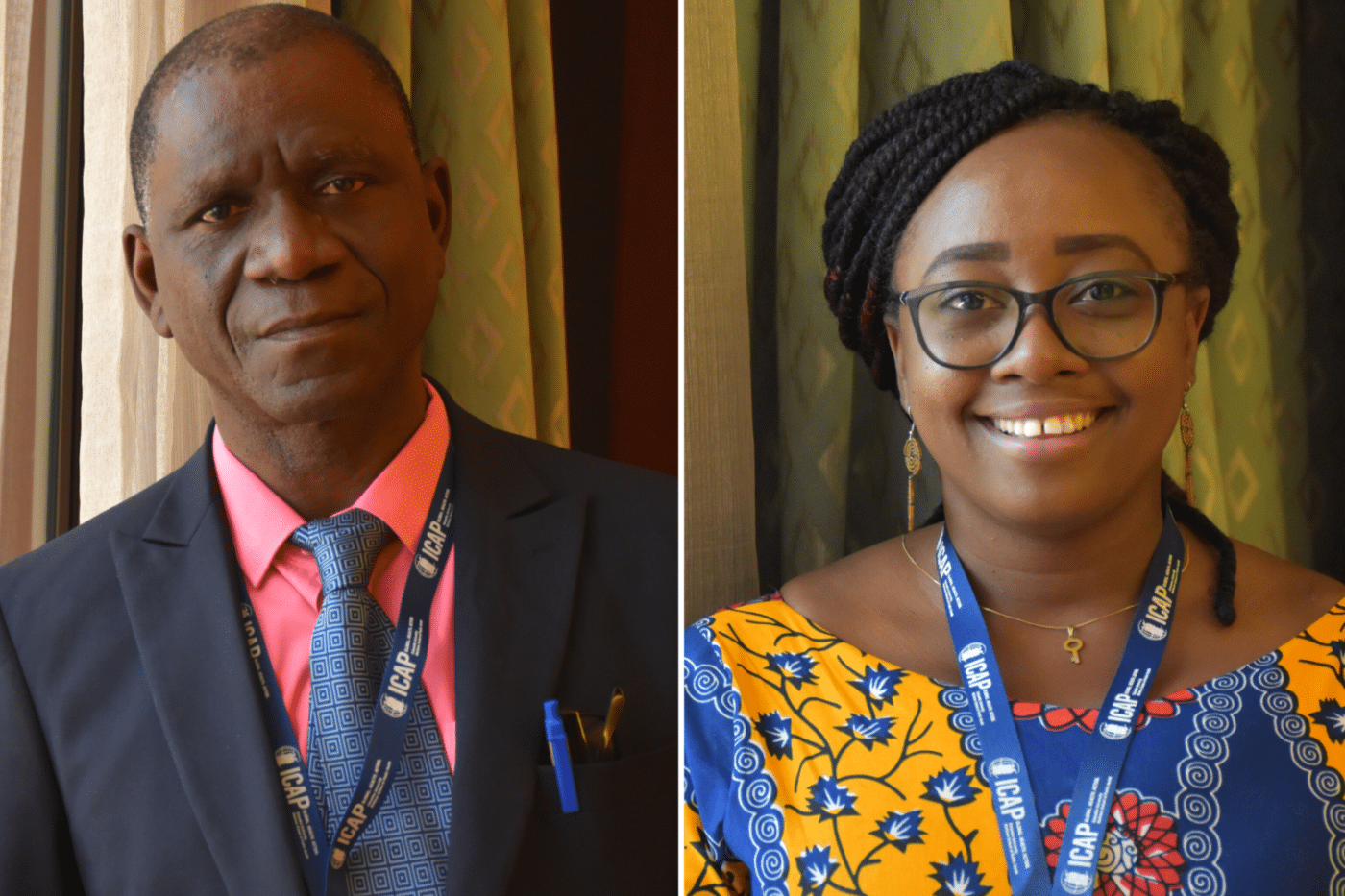
Idrissa Songo (left), is an electrical engineer by training as well as a project management specialist and the founder and executive director of the Network of HIV Positives in Sierra Leone (NETHIPS).
Alren Vandy MD, MPH, (right) is the national antiretroviral therapy (ART) coordinator for the National HIV/AIDS Control Programme for Sierra Leone’s Ministry of Health and Sanitation.
Sierra Leone is one of three new countries that joined CQUIN in September 2019. Dr. Vandy and Mr. Songo attended the third annual CQUIN meeting in Johannesburg, South Africa in November 2019 as representatives of Sierra Leone, where they shared their thoughts on joining the network, why differentiated service delivery (DSD) is a priority for Sierra Leone’s national HIV program, and key takeaways from their first CQUIN meeting.
What is your background and current role?
AV: I completed medical school six years ago in Russia and later pursued my master’s in public health in Ghana. I returned home to Sierra Leone because I am very passionate about both improving access to sexual and reproductive health and strengthening health systems—I see my role as the national ART coordinator for the National HIV/AIDS Control Programme (NACP) as an extension of both of those ambitions. I serve as the lead clinician responsible for the management of HIV/AIDS and linkage to care at the NACP, providing technical leadership in the planning, development, implementation, and monitoring of HIV services, as well as clinical supervision and oversight for staff in all ART clinics.
One of my favorite parts about my role is working directly with community members. I partake in sessions with the Network of HIV Positives in Sierra Leone (NETHIPS) to hear questions and input from recipients of care and provide them with information. Information is very powerful—it shows people living with HIV that providers care, it helps to de-stigmatize HIV, and it empowers recipients of care to be heard in the design and delivery of HIV services.
IS: I am an engineer by profession, now turned administrator. While I was working at the Sierra Leone Port Authority as an engineer it came to my attention that I could do more to contribute to the HIV response in my country. At the time, the development sector was not taking HIV seriously, and we needed to galvanize support and help people understand the reality of the situation.
In my current role as the founder and executive director of NETHIPS, I work directly with community members and people living with HIV, facilitating care and support groups in Sierra Leone in line with the National AIDS Secretariat in order to improve HIV services and advocate for the needs of PLHIV.
Why is Sierra Leone starting to focus on DSD in its national HIV programming?
AV: We want to improve the quality of our care and be more client-centered. In Sierra Leone, many people who require care must travel very far to receive it, and proper roads and transportion are often inaccessible. The health centers can be congested since we have a limited health workforce. Our goals in piloting DSD are to strengthen human resources for health and provide more options for people doing well on treatment, hopefully decongesting health centers.
IS: Right now, there are some activities in Sierra Leone that could be considered DSD models, but they are fragmented and unstructured. We would like to get these activities on a proper track and begin implementing and measuring DSD because we believe it will not only lift the burden off our health centers, but most importantly improve the lives of people living with HIV.
How are you hoping to begin implementing DSD in Sierra Leone? Are there any models that have stood out to you?
AV: The most important thing for us is to start giving people living with HIV a choice. Since we are at the very initial stages of DSD implementation we want to prioritize people doing well on treatment and ensure they have access to care that works best for them. We are leaning toward three-month multi-month scripting to start, and will see what kind of impact that has. Another approach we are considering is to involve community health workers in conducting community ART refills. Not only implementing a facility-based individual model but creating more options for those who cannot reach facilities, ensuring those individuals get their medication.
Because our human resources for health are limited and our clinics are typically overwhelmed, we would like to move away from facility-based models. However, the most important thing is for us to provide recipients of care with more options and make sure we are effectively involving the community.
IS: I think it’s key for us to not focus on one specific model. What we are understanding through CQUIN is that DSD implementation must be context specific. We must look at models that fit with the health system and are appreciated by ROC. Anything we implement will likely be in a phased approach rather than an immediate rollout, because if not, we might have gaps in our understanding of how a model is performing. Through a combined phase approach with continuous community engagement, we hope to come up with what works best for us.
Another area that is key to implementing DSD is continued commitment at all levels—government, partners, community members. Our existing partnerships are strong, and we hope to leverage these by sharing what we have learned about DSD and building momentum to coordinate a special DSD technical working committee, working with partners to shift the dynamics of the HIV response in our country.
What are your impressions of your first CQUIN annual meeting?
AV: It has been great. I’ve met a lot of dedicated people from different countries through networking, and I hope to contact them in the future to learn about their innovative ideas and initiatives in improving HIV care. It is a very strong learning platform. For a country like Sierra Leone that is just starting to pilot DSD initiatives, it is a huge advantage to be here and learn from countries who have been refining DSD for some time. We can again look at their lessons-learned and possibly fast-track our activities to keep up with the pace.
I look forward to starting to implement back home and sharing what we have learned at next year’s meeting.
IS: Honestly, the organization of the meeting is just powerful; from the moderation to the presentations—it’s a great learning opportunity. At the Tools Lab session, we learned what other countries are doing to acquire data on DSD, and it was very valuable for us to access that information.
Another thing that really impresses me about CQUIN is the South-to-South learning. I’m hoping Sierra Leone can participate in a visit in the future, since there is huge opportunity to learn from DSD programs that are working in other countries. We truly appreciate joining this network, especially at this particular time when there are so many best practices to draw upon.
Learn about ICAP’s broader portfolio of work in Sierra Leone.
The CQUIN 3rd Annual Meeting took place in Johannesburg, South Africa from November 10-14, 2019.